Children's Asthma and COVID-19 | CMI Health
COVID-19 and Child Asthma
It has been well established that COVID-19 is an aggressive respiratory virus with the ability to cause systemic infection. For those who already struggle with respiratory disorders, the recent pandemic caused great alarm. Though most areas in the United States are emerging from the COVID-19 pandemic, authorities and researchers have voiced new concerns regarding the development and rise in new COVID-19 variants and the potential of these variants to have a higher affinity for children (Reuters, 2021). While it is too early for conclusive data to be presented, precaution must be taken.
According to the CDC, those diagnosed with previous medical conditions, such as asthma or heart disease, are at an increased risk of developing severe illness. For children, whose lungs are still developing into their teenage years, severe lung infections can lead to long-term lung damage. The risk factor is even greater for those diagnosed with Asthma (CDC, 2021).
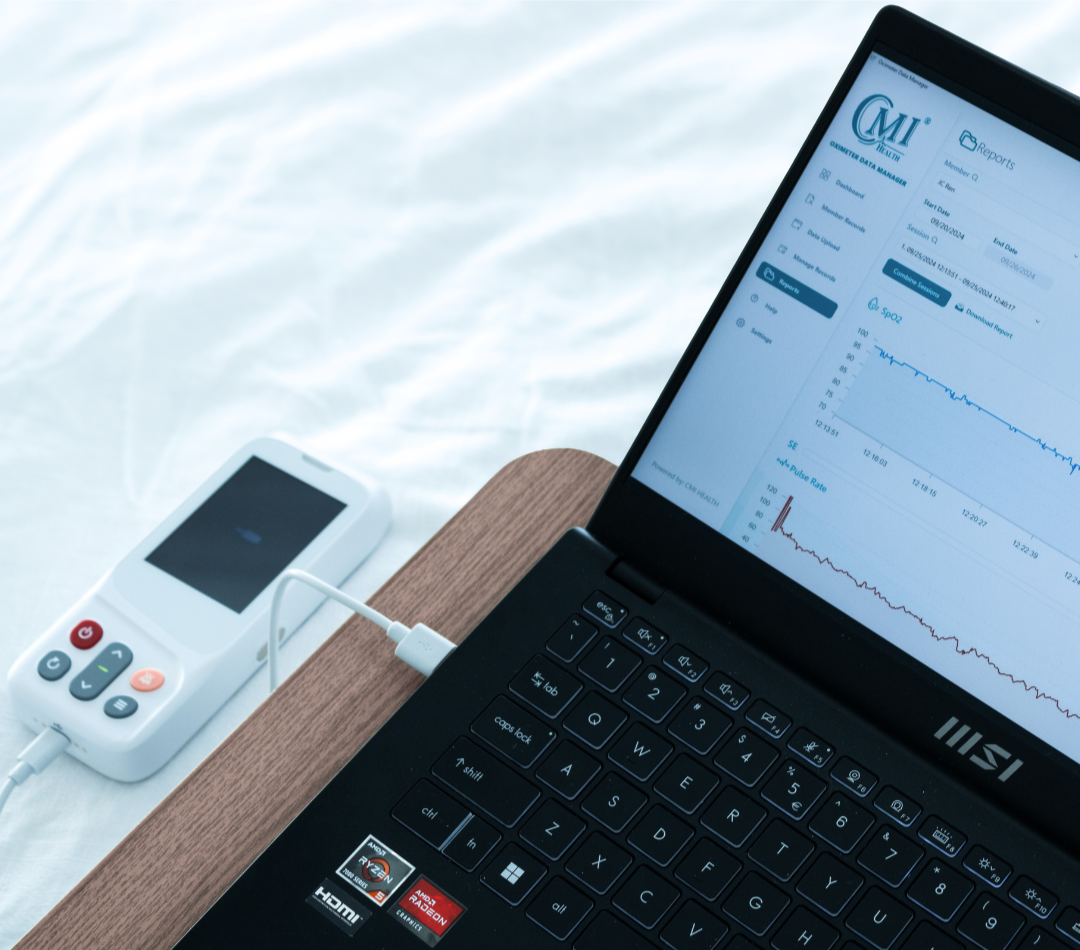
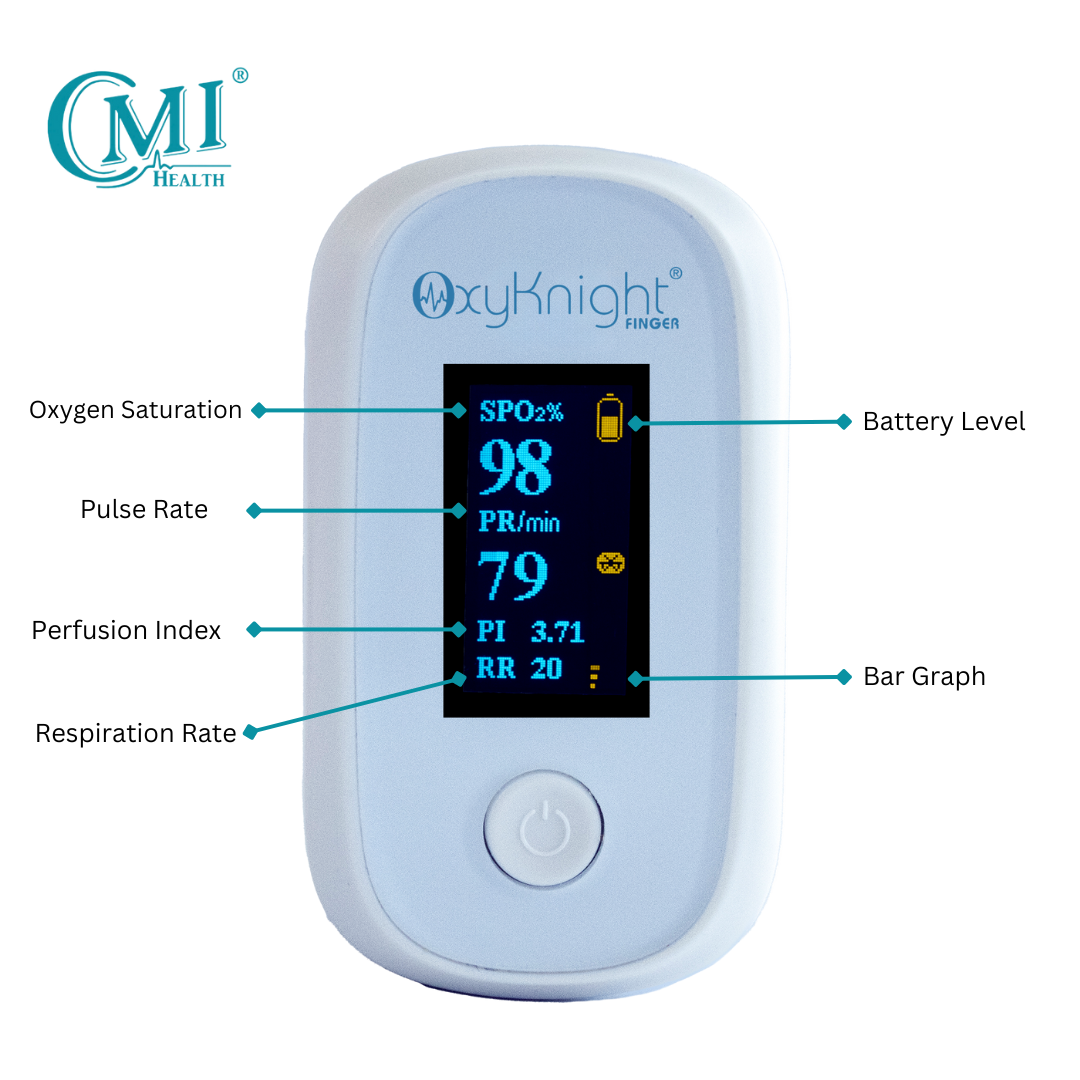
Taking precautionary steps to protect children may result in earlier infection recognition. Pulse Oximeters allow users to monitor lung function by tracking oxygen levels on the go or continuously. Though a child may seem fine, their oxygen levels may be dropping due to an infection that has not yet caused visible symptoms. COVID 19 has been shown to cause silent hypoxia, a damaging and dangerous side effect that presents little to no symptoms in the early stages (ScienceDaily, 2020). This is particularly dangerous for those who have asthma and may be accustomed to lung irritation. Tracking oxygen levels is a safe and non-invasive method of monitoring your child's everyday health.
What is Silent Hypoxia?
In humans, hypoxia can be generally defined as an overall oxygen deficiency in the blood stream and tissues. In the early stages of the Covid-19 pandemic, it was determined that the virus was capable of causing silent hypoxia in its early stages. This news was frightening due to the seemingly undetectable nature of such a side effect. Unlike common pneumonia, which leads to visible shortness of breath, chest pain, and sometimes coughing, Covid-19 pneumonia initially causes imperceptible oxygen deprivation (Teo, 2020).
The outstanding issue with this type of illness is that by the time the patient shows signs of sickness, they have already begun to develop moderate to severe pneumonia (Teo, 2020). For children afflicted with Asthma, such an infection can be extremely dangerous. To avoid long term lung damage or other worse symptoms, monitoring your child’s everyday lung health can provide parents with early warning signs of infection. According to one recently published scientific article, at-home pulse oximetry devices “…may lead to a significant increase in the early detection of silent hypoxia, and hence identification of the onset of COVID-19 pneumonia” (Teo, 2020).
Tracking Child Lung Health
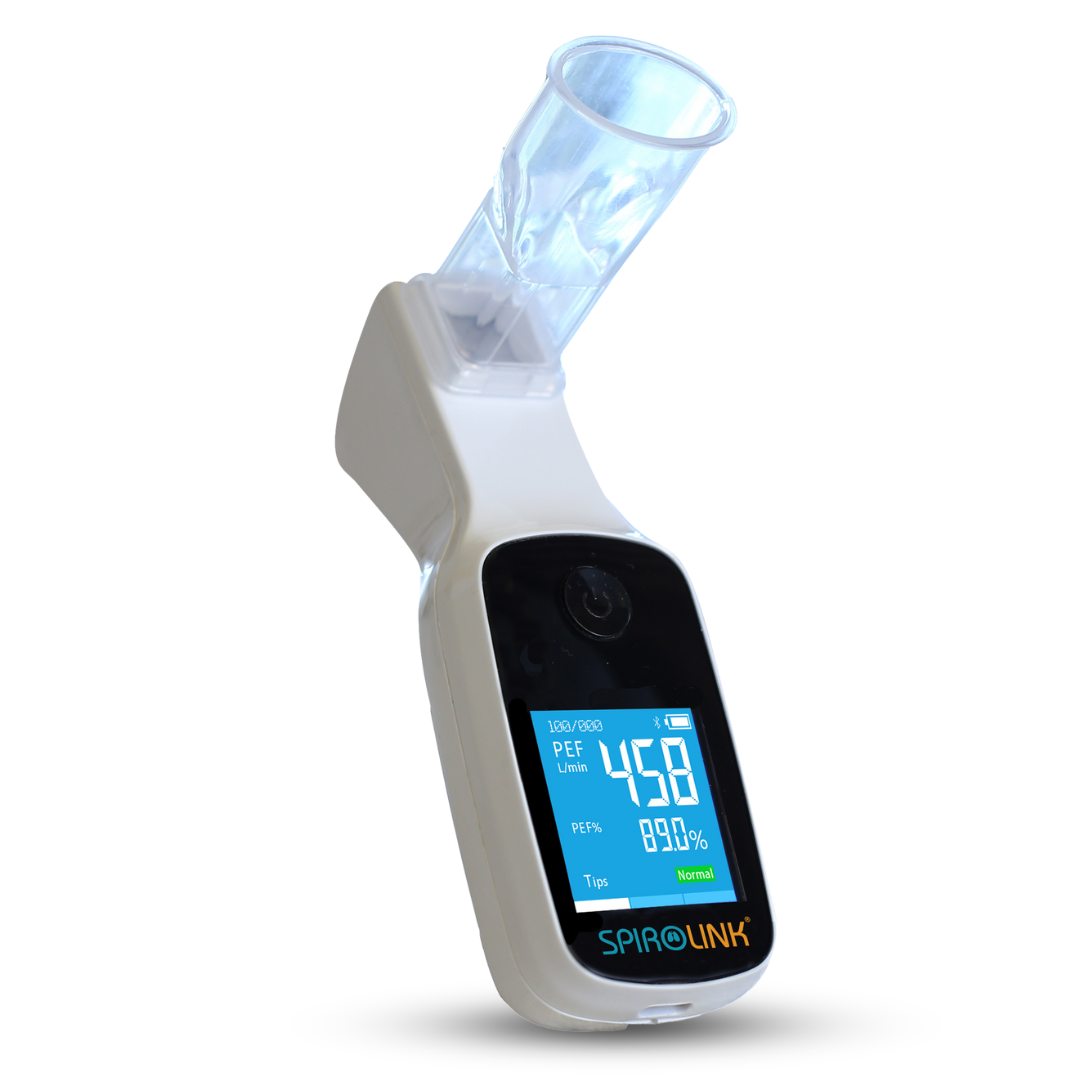
Spirometry devices that track and record lung health and function are also useful tools for measuring overall pulmonary lung function and respiratory health. SpiroLink, a digital spirometer with a user-friendly mobile app, is an ideal candidate for monitoring asthma in both children and adults. Considering the high cost of hospital equipment and doctor visits, having access to affordable and portable at-home clinical grade medical devices can make a huge difference in the long-term treatment of chronic illnesses.
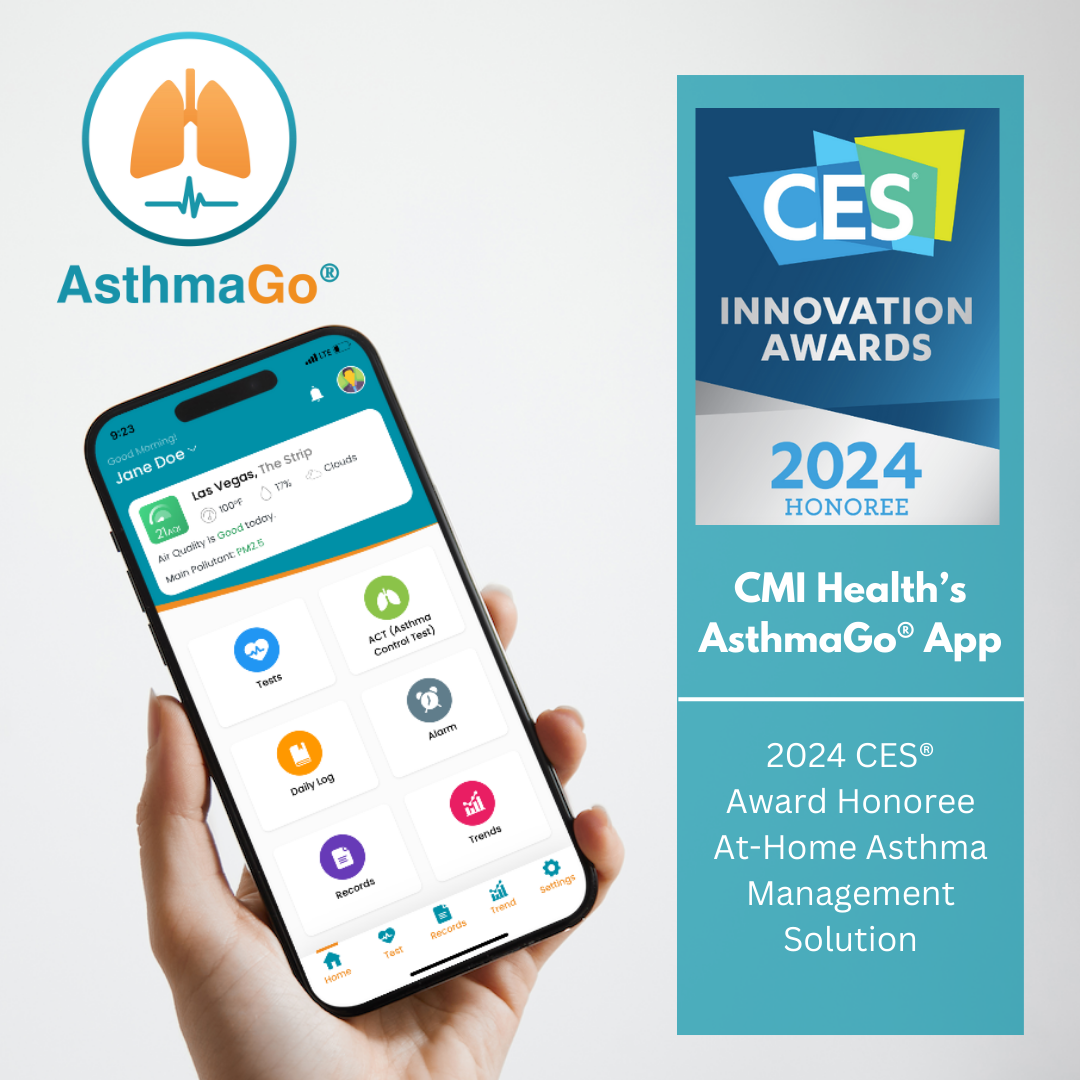
CMI’s Telehealth Solution for Children’s Asthma Management at-home is great for monitoring, tracking, and managing Asthma. Powered by CMI Health's home use spirometer, continuous oximetry monitor, and cloud-based mobile App, Tele-CAS helps to connect patients with their doctors remotely and achieve better outcomes. This telemedicine solution allows parents flexibility in monitoring their child’s condition while ensuring their progress is accurately tracked.
For more information, feel free to contact us at info@cmihealth.com!































Leave a comment